Psoriasis is not just about skin rashes and itchiness, but may also present risks with other health issues (a.k.a comorbidities). Find out which ones you may be at risk for, and how to deal with them — brought to you by Not Alone with Psoriasis, a blog by Novartis — featuring dermatologist Dr Khor Yek Huan.
Unpacking the Meaning of “Comorbidity” in the Context of Psoriasis…
Living with psoriasis can be one of the most challenging experiences in one’s life. We should feel comfortable and confident when we go out in the world and interact with other people, but painful, itchy, thick red patches called plaques covering visible areas of our body make us self-conscious. And this in turn leads to anxiety or depression.

It is often said that psoriasis is not just a ‘skin-deep disease’. What we mean when we say that, is, psoriasis is an auto-immune disorder that affects our health from the inside out. Not only are psoriasis patients (roughly 2-3% of the population) feeling the emotional and psychological burdens of living with their lifelong skin condition, they are often vulnerable to other health risks that are co-morbid with psoriasis1.
Comorbidity is defined as the co-occurrence of two or more disorders in the same individual at the same point in time2. These are medical conditions that often co-exist simultaneously as another condition (not necessarily because of it)3.
You could have a comorbid condition because of underlying shared systemic factors, lifestyle choices, or treatment side effects4. For example, because you have psoriasis, your immune system is at risk of cardiovascular disease or diabetes. Or, because you have severe psoriasis, and your lifestyle choices have not allowed you to manage it well, you may have developed depression. Genetically, you may be pre-disposed to developing psoriatic, causing joint pain and deformities.5
Comorbidities traditionally associated with psoriasis are: metabolic syndrome (MetS), atherosclerosis, psoriatic arthritis (PsA), inflammatory bowel disease (IBD), uveitis, and psychological and psychiatric disorders6. More recent studies have demonstrated a link between psoriasis and metabolic syndrome, cardiovascular disease, fatty liver, lymphoma, and sleep apnea7.
Finding out which comorbid diseases you are at risk for is helpful for a more holistic approach to your long-term treatment, and better quality of life. If needed, your dermatologist may refer you to primary care specialists.8 Being aware of your risks allows you to make better-informed lifestyle choices.
6 Prevalent Comorbidities to Look Out for If You Have Psoriasis

1. Metabolic Syndromes and its Components
Evidence suggests that psoriasis patients are at a higher risk (20-50% prevalence rate) of developing metabolic syndrome (MetS)9. MetS is a cluster of at least 3-5 syndromes occurring together that are impacted by energy utilization and storage10.
Based on The National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATP III) and World Health Organisation (WHO) criteria, metabolic abnormalities associated with psoriasis are: abdominal obesity, hypertension, atherogenic dyslipidemia, type 2 diabetes, insulin resistance, and nonalcoholic fatty liver disease11. Having MetS is a strong predictor of developing cardiovascular disease12.
Abdominal obesity is defined as having a waist circumference of greater than 102 centimeters (40 inches) in men or 88 centimeters (35 inches) in women13. Psoriasis patients also have a higher incidence of general obesity, which is defined as having a body mass index of greater than 25kg/m2 for Asian people14.
Unfortunately, obese patients with psoriasis are more likely to experience negative side effects to medications. In addition, they are less likely to respond favorably to psoriasis treatments. It’s important to know that increased body fat is associated with higher levels of inflammation in the body, which might put you at a higher risk of developing more severe psoriasis15.
Losing weight has been shown to improve psoriasis symptoms and help make treatments more effective16. However, any weight loss should be carried out under the advice and supervision of a doctor. Patients are generally recommended to exercise regularly and adopt healthy eating habits.

Diabetes Mellitus is type 2 diabetes. People with severe psoriasis are 46% more likely to develop Type 2 diabetes than people without psoriasis17. Look out for the following symptoms18: unusual thirst, hunger, blurred vision, fatigue, or frequent urination, recurring skin, gum, or bladder infections, cuts and bruises that are slow to heal, tingling or numbness in the hands or feet.
Early screening, diagnosis and treatment is crucial. Allowing Type 2 diabetes to go unchecked puts patients at risk for artherosclerosis, ischemic heart disease (IHD), stroke, end stage renal failure, peripheral neuropathies and blindness19.
Here are diagnostic thresholds to look out for: average blood glucose (A1C) levels 5.7% to 6.4% is prediabetes, whereas A1C levels 6.5% or higher is diabetic. Normal fasting blood glucose (FPG) 100mg/dl to 125mg/dl is prediabetes, conversely FPG 125mg/dl or higher is diabetic. We should maintain A1C levels of less than 5.7% and FPG of less than 100mg/dl20.
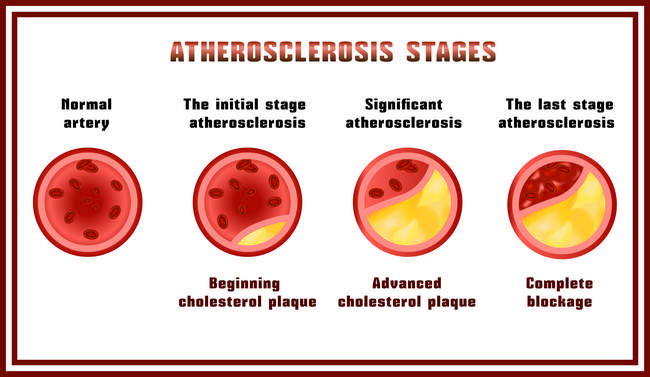
2. Atherosclerosis and Related Complications
One of the common comorbidities with psoriasis is atherosclerosis, essentially, a disease where plaque builds up inside your arteries21. This leads to serious medical complications, particularly like ischaemic heart disease (coronary artery disease), cerebrovascular disease (stroke) and peripheral vascular disease (blood circulation disorder)22.
If you have a family history of psoriasis and atherosclerosis, do check for symptoms of cerebrovascular disease: limb weakness, numbness, facial asymmetry, slurring of speech, unstable gait,23 and symptoms of peripheral vascular disease: calf pain related to walking distance (intermittent claudication), painful non-healing of ulcers over toes24.
Cardiovascular disease (CVD) is a set of heart and blood vessel diseases including coronary artery disease and heart attacks25. A population based study in UK has shown that the greater the severity of psoriasis, the stronger the association between psoriasis and cardiovascular disease.26 Patients with severe psoriasis also have a higher risk of cardiovascular mortality, independent of common risk factor27. Cardiovascular disease symptoms to look out for are: chest pains, chest discomfort, shortness of breath, decreased effort tolerance, and dizziness28.
When you treat your psoriasis autoimmune disorder by suppressing systemic inflammation with biological agents, this ameliorates risk factors for CVD29. Lifestyle medications and periodic blood investigations (such as for metabolic syndrome) are recommended.
In addition, if you have psoriasis you should consult a physician if you are experiencing any of the above-mentioned symptoms immediately. Most physicians are unaware of the connection between psoriasis & cardiovascular disease30.
3. Psoriatic Arthritis
According to the National Psoriasis Foundation, up to 30% of psoriasis patients develop psoriatic arthritis (PsA)31. PsA characterized by swelling, pain, and stiffness of the joints, ligaments, and tendons32.
Look out for symptoms of: fatigue, joint stiffness first thing in the morning or after a resting period, swollen fingers or toes resembling sausages, tenderness/pain/swelling of tendons and joints, and nail changes (if your nail separates from the nail bed, or if you get pitted nails that look like fungus infections)33.
There is often a delay in diagnosing PsA and administering treatment. As a result, PsA patients may suffer from progressive structural joint damage and permanent deformities which severely impair their day-to-day activities and affect their quality of life.
PsA usually occurs between ages 30 and 50 years of age. If you have psoriasis and experience joint aches and pains, you should consult your dermatologist and doctor without delay. If you are diagnosed with psoriatic arthritis, you should consider seeing a rheumatologist (a doctor who specializes in arthritis).
There is no definitive test for PsA. Your doctor will need to assess you by looking at your medical history, especially your history with psoriasis. He/she may perform a physical examination, requisition blood tests, MRI’s and X-Ray’s of your joints that have symptoms to diagnose PsA.
The primary goals in managing PsA comorbidity are to improve your quality of life, reduce the structural progression of joint damage, and reduce the risk of deformities. To read more about psoriatic arthritis, please visit our blog.
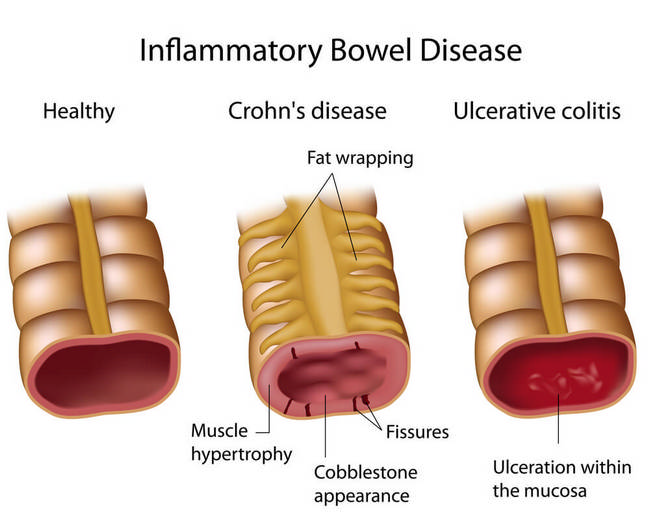
4. Inflammatory Bowel Disease
Numerous findings show that due to shared inflammatory pathways between psoriasis and inflammatory bowel disease (IBD), there is an increase in incidence rate of comorbidities between the two34 (IBD includes Crohn’s Disease, which affects the small bowel and Ulcerative colitis, which affects the large intestine35).
Look out for symptoms of diarrhoea, abdominal cramping, bloody stools, weight loss, and anemia36.
Moreover, patients with psoriasis and concomitant IBD have a higher rate of other comorbidities (seronegative arthritis, thyroiditis, diabetes and lymphoma) than patients with only psoriasis37.
If you experience severe symptoms, consult your doctor immediately. When necessary, make an appointment to see a gastroenterologist. A diagnosis will be made via: blood test, stool sample, endoscopic and imaging procedures38.
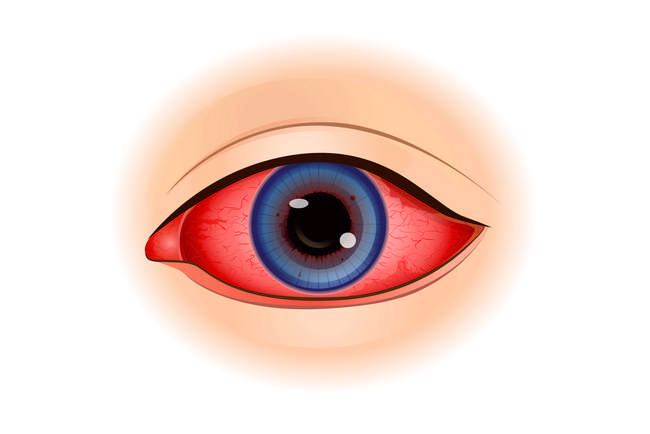
5. Uveitis
People who have psoriasis or psoriatic arthritis are slightly more likely to develop uveitis than an average person, uveitis refers to several diseases related to the inflammation of the eye39. It affects the middle layer of tissue in the eye wall40.
Symptoms to watch out for are: eye redness, eye pain, light sensitivity, dark floating spot in your field of vision, and blurred vision (in one of both eyes)41.
This primarily affects people ages 20 to 50. It requires specific treatment, so consult an eye doctor if you do have symptoms. Seek an ophthalmologist/ocular immunologist near you.

6. Psychological and Psychiatric Disorders
Last, but not least, psychological and psychiatric disorders are invisible comorbidities for psoriasis sufferers.42 These are so often overlooked and difficult to talk about. The physical, emotional, and social impact of psoriasis on a patient’s quality of life can be similar or worse than that of ischemic heart disease, cancer, arthritis, and diabetes mellitus.
If you have psoriasis or knows someone with psoriasis, look out for these signs: feeling worried or empty for long durations, loss of interest in activities they once enjoyed, feeling tired all the time, unable to concentrate, slow in making decisions, restless or irritable, change in eating/sleeping/other habits, thoughts of death or suicide, attempting suicide43. This is the worst-case scenario that affects depressed patients, as it could be fatal.
These comorbidities threaten to complicate ongoing treatment for psoriasis patients, because patients could be less compliant to treatment regiments. They could be further deprived from social activities, and marred participation in their own careers could result in unemployment. These patients then become more of a burden to their families.
Psoriasis is a complex and difficult disease. Being bottled up inside can add to your stress and worsen your symptoms. Share your feelings and problems with your family and friends.
Be more open and honest about your condition, especially with your doctor. It’s important for your doctor to be aware of the total impact psoriasis has on you.
Joining a psoriasis patient’s support group could prove helpful. You are not alone with the disease. Learn and share experiences with other people who are living full lives with psoriasis every day.
Learn some relaxation techniques e.g. exercise and yoga to lower stress.
Talk to a psychiatrist if you have any of the symptoms mentioned above. The psychiatrist will help assess your condition by talking to you about your thoughts, feelings, and behavioural patterns. You may be asked to fill out assessment questionnaires.
Visit our Facebook page to find out more information about psoriasis.
Read stories like this and more about psoriasis on our MyPsoriasis blog.
Visit #Ask4Clear and find the best dermatologist near you today!
If you enjoyed this article, read Biologic Treatment For Psoriasis: 4 Tips You Should Know
References
- 1 https://www.psoriasis.org/about-psoriasis
- 2 https://www.sciencedirect.com/topics/neuroscience/comorbidity
- 3 https://www.merriam-webster.com/dictionary/comorbid
- 4, 8 http://www.dermatologytimes.com/psoriasis/psoriasis-comorbidities-101
- 5 https://ghr.nlm.nih.gov/condition/psoriatic-arthritis#genes
- 6, 7 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4323693/
- 9, 10, 11, 12 https://www.sciencedirect.com/science/article/pii/S0738081X17301591
- 13, 14 https://www.hsph.harvard.edu/obesity-prevention-source/obesity-definition/abdominal-obesity/
- 15 https://www.psoriasis.org/about-psoriasis/associated-conditions/does-obesity-lead-to-psoriasis
- 16 https://www.psoriasis.org/about-psoriasis/treatments/alternative/diet-supplements
- 17, 18 https://www.psoriasis.org/media/press-releases/psoriasis-tied-higher-risk-type-2-diabetes
- 19 https://www.sciencedirect.com/topics/medicine-and-dentistry/complications-of-diabetes-mellitus
- 20 http://www.diabetes.org/diabetes-basics/diagnosis/
- 21 https://www.nhlbi.nih.gov/health-topics/atherosclerosis
- 22, 30 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4000177/
- 23 http://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Cerebrovascular-Disease
- 24 https://www.cardiosmart.org/Heart-Conditions/Peripheral-Vascular-Disease
- 25 http://www.heart.org/HEARTORG/Conditions/What-is-Cardiovascular-Disease_UCM_301852_Article.jsp#.WzHK8aczbIU
- 26 Langan SM, Seminara NM, Shin DB, Troxel AB, Kimmel SE, Mehta NN, et al. Prevalence of metabolic syndrome in patients with psoriasis: A population-based study in the United Kingdom. J Invest Dermatol. 2012;132:556–562
- 27 Mehta NN, Yu Y, Pinnelas R, Krishnamoorthy P, Shin DB, Troxel AB, et al. Attributable risk estimate of severe psoriasis on major cardiovascular events. Am J Med. 2011;124:775.e1–775.
- 28 https://www.webmd.com/heart-disease/guide/heart-disease-symptoms#1
- 29 Arumugam R, McHugh NJ. Mortality and causes of death in psoriatic arthritis. J Rheumatol. 2012;89(Suppl):32–35
- 31, 32 https://www.psoriasis.org/about-psoriasis/related-conditions
- 33 https://www.psoriasis.org/about-psoriatic-arthritis#diagnosed
- 34 https://www.ncbi.nlm.nih.gov/pubmed/19207663/
- 35 http://www.crohnscolitisfoundation.org/what-are-crohns-and-colitis/what-is-crohns-disease/
- 36 https://www.crohnsandcolitis.org.uk/about-inflammatory-bowel-disease/what-are-the-symptoms
- 37 Binus AM, Han J, Qamar AA, Mody EA, Holt EW, Qureshi AA, et al. Associated comorbidities in psoriasis and inflammatory bowel disease. J Eur Acad Dermatol Venereol. 2012;26:644–650
- 38 https://www.mayoclinic.org/diseases-conditions/inflammatory-bowel-disease/diagnosis-treatment/drc-20353320
- 39, 40 https://www.psoriasis.org/advance/uveitis-eye-inflammation-linked-to-psoriasis-psoriatic-arthritis
- 41 https://www.mayoclinic.org/diseases-conditions/uveitis/symptoms-causes/syc-20378734
- 42 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4928455/
- 43 https://www.psoriasis.org/life-with-psoriasis/depression

 Tue-Fri 10:00-20:00
Tue-Fri 10:00-20:00
 +604-638 3393 / +6010-399 7713
+604-638 3393 / +6010-399 7713
 B-2-1, Bay Avenue, Bayan Lepas
B-2-1, Bay Avenue, Bayan Lepas